Source: www.aultman.com/hgcontent.asp?chunkiid=37409 OverviewOsteopathy originated as a 19th century alternative medical approach focusing on physical manipulation. Today, osteopathic physicians study and practice the same types of medical and surgical techniques as conventional medical doctors. Some of osteopathy's original techniques still persist, however; these, taken together, are called osteopathic manipulation (OM). OM is less well-known to the public than
chiropractic spinal manipulation, but it has shown promise for many of the same conditions: for example, back pain and tension headaches.
History of Osteopathic ManipulationOsteopathic medicine was founded in 1874 by Andrew Taylor Still, a U.S. physician. Physicians educated in this method were called doctors of osteopathy, or D.O.s. Subsequently, however, schools of osteopathic medicine became integrated with conventional medical schools, and today the license of D.O. is legally equivalent to that of M.D.
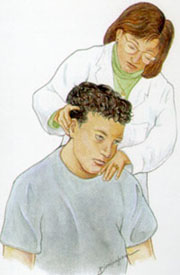
Forms of Osteopathic ManipulationOsteopathic and
chiropractic techniques overlap, but they are not identical. As a general rule, chiropractors focus most of their attention on the spine, while osteopathic practitioners devote more of the their efforts to the manipulation of soft tissues and joints outside the spine. Another general difference is that chiropractic spinal manipulation tends to make use of rapid short movements (spinal manipulation, which is a high-velocity, low-amplitude technique), while OM typically concentrates on gentle, larger movements (mobilization, which is a low-velocity, high-amplitude technique). But neither of these distinctions is absolute, and many chiropractic and osteopathic methods do not fit neatly into these categories.
There are several specific osteopathic techniques in wide use, many of which are named after their founders. Some of the more popular are Greenman muscle-energy, Jones counterstrain (also known as strain-counterstrain), myofascial release, and cranial-sacral therapy (formally known as osteopathy in the cranial field).
Greenman Muscle-energy TechniqueGreenman muscle-energy technique involves bending a joint just up to the point where muscular resistance to movement begins (“the barrier”), and then holding it there while the patient gently resists. The pressure is maintained for a few seconds and then released. After a brief pause to allow the affected muscles to relax, the practitioner then moves the joint a little farther into the barrier, which will usually have shifted slightly toward improved mobility during the interval.
Strain-counterstrain Technique (Jones Counterstrain)Strain-counterstrain technique (Jones counterstrain) involves finding tender points and then manipulating the joint connected to them in order to find a position where the tenderness decreases toward zero. Once this precise angle is found, it is held for 90 seconds and then released. Like muscle-energy work, strain-counterstrain progressively increases range of motion and, it is hoped, decreases muscle spasm and pain.
Myofacial ReleaseMyofacial release focuses on the fascial tissues that surround muscles. The practitioner first positions the painful area either at the edge of the barrier to movement or, alternatively, at the opposite extreme (the area of greatest comfort). Next, while the patient breathes slowly and easily, the practitioner palpates the fascial tissues, looking for a subtle sensation that indicates the tissues are ready to “unwind.” After receiving this indication, the practitioner then helps the tissue to follow a pattern of spontaneous movement. This process is repeated over several sessions until a full release is achieved. Myofascial release is said to be especially useful in pain conditions that have persisted for months or years.
Cranial-sacral TherapyCranial-sacral therapy, more properly called cranial osteopathy (or just cranial for short), is a very specialized technique based on the scientifically unconfirmed belief that the tissues surrounding the brain and spinal cord undergo a rhythmic pulsation. This “cranial rhythm” is supposed to cause subtle movements of the bones of the skull. A practitioner of cranial-sacral therapy gently manipulates these bones in time with the rhythm (as determined by the practitioner’s awareness), in order to repair “cranial lesions.” This therapy is said to be helpful for numerous conditions ranging from headaches and sinus allergies to multiple sclerosis and asthma. However, many researchers have serious doubts that the cranial rhythm even exists.
11What is Osteopathic Manipulation Used For?Osteopathic manipulation is primarily used to treat
musculoskeletal pain conditions, such as
back pain,
shoulder pain, and
tension headaches. OM is often said to be specifically effective for conditions that have persisted for some time, as opposed to chiropractic spinal manipulation, which, according to this view, is most effective for treatment of injuries that have occurred recently. However, there is no meaningful scientific support for this belief.
Some advocates of OM believe that it has numerous additional benefits, including the enhancement of
overall health and well-being.
Possible Effects of OMMost studies of OM have involved its potential use for various pain conditions.
In a study of 183 people with
neck pain, use of osteopathic methods provided greater benefits than standard physical therapy or general medical care.
12 Participants receiving OM showed faster recovery and experienced fewer days off work. OM appeared to be less expensive overall than the other two approaches; however, researchers strictly limited the allowed OM sessions, making direct cost comparisons questionable. Another study evaluated a rather ambitious combined therapy for the treatment of chronic pain resulting from whiplash injury (craniosacral therapy along with Rosen Bodywork and Gestalt psychotherapy).
13 The results failed to find this assembly of treatments more effective than no treatment.
In a 14-week, single-blind study of 29 elderly people with
shoulder pain, real OM proved more effective than placebo OM.
1 Although participants in both groups improved, those in the treated group showed relatively greater increase in range of motion in the shoulder.
In another study, 24 women with
fibromyalgia were divided into five groups: standard care, standard care plus OM, standard care plus an educational approach, standard care plus moist heat, and standard care plus moist heat and OM.
2 The results indicate that OM plus standard care is better than standard care alone, and that OM is more effective than less specific treatments, such as moist heat or general education. However, because this was not a blinded study (participants knew which group they were in), the results can’t be taken as reliable.
A study of 28 people with
tension headaches compared one session of OM against two forms of sham treatment, and found evidence that real treatment provided a greater improvement in headache pain.
3Although OM has shown some promise for the treatment of
back pain,
4,5 one of the best-designed trials failed to find it a superior alternative to conventional medical care. In this 12-week study of 178 people, OM proved no more effective than standard treatment for back pain.
6 Another study, this one enrolling 199 people and following them for 6 months, also failed to find OM more effective than fake OM.
14 This study also included a no-treatment group. Both real and fake OM were more effective than no treatment.
A much smaller study reportedly found that muscle-energy technique enhances recovery from back pain, but this study does not appear to have used a meaningful placebo treatment.
15Some studies have evaluated the potential benefits of OM for speeding healing in people recovering from
surgery or serious illness. The best of these studies compared OM against light touch in 58 elderly people hospitalized for pneumonia.
7 The results indicate that use of osteopathy aided recovery.
In a much less meaningful study, OM was compared to no treatment in people recovering from knee or hip surgery.
8 While the people receiving OM recovered more quickly, these results mean very little, since, as noted above, any form of attention should be expected to produce greater apparent benefits than no attention.
A similarly weak study suggests that OM might also be helpful for people hospitalized with
pancreatitis.
9A small study found some evidence that OM might be helpful for childhood
asthma.
16Finding a Qualified Practitioner of Osteopathic ManipulationAlthough there are many licensed doctors of osteopathic medicine (DOs), most practice conventional medicine and do not specialize in OM. Some do, and many of those have been certified by the American Osteopathic Board of Neuromusculoskeletal Medicine.
In addition, many physical therapists and massage therapists use some osteopathic techniques, with variable amounts of training.
Safety of Osteopathic ManipulationMost forms of OM, because of their gentle nature, are believed to be quite safe. However, mild short-term pain may occur immediately following treatment.
10 In addition, some osteopathic practitioners use the high-velocity thrusts common to chiropractic, and might therefore incur some slight safety risks. Overall, OMT is very safe.
References
1. Knebl JA, Shores JH, Gamber RG, et al. Improving functional ability in the elderly via the Spencer technique, an osteopathic manipulative treatment: a randomized, controlled trial. J Am Osteopath Assoc. 2002;102:387–396.
2. Gamber RG, Shores JH, Russo DP, et al. Osteopathic manipulative treatment in conjunction with medication relieves pain associated with fibromyalgia syndrome: results of a randomized clinical pilot project. J Am Osteopath Assoc. 2002;102:321–325.
3. Hoyt WH, Shaffer F, Bard DA, et al. Osteopathic manipulation in the treatment of muscle-contraction headache. J Am Osteopath Assoc. 1979;78:322–325.
4. Newswanger DL, Patel AT, Ogle A. Osteopathic medicine in the treatment of low back pain. Am Fam Physician. 2000;62:2414–2415.
5. Koes BW, Assendelft WJ, van der Heijden GJ, et al. Spinal manipulation for low back pain. An updated systematic review of randomized clinical trials. Spine. 1996;21:2860–2873.
6. Andersson GBJ, Lucente T, Davis AM, et al. A comparison of osteopathic spinal manipulation with standard care for patients with low back pain. N Engl J Med. 1999;341:1426–1431.
7. Noll DR, Shores JH, Gamber RG, et al. Benefits of osteopathic manipulative treatment for hospitalized elderly patients with pneumonia. J Am Osteopath Assoc. 2000;100:776–782.
8. Jarski RW, Loniewski EG, Williams J, et al. The effectiveness of osteopathic manipulative treatment as complementary therapy following surgery: a prospective, match-controlled outcome study. Altern Ther Health Med. 2000;6:77–81.
9. Radjieski JM, Lumley MA, et al. Effect of osteopathic manipulative treatment on length of stay for pancreatitis: a randomized pilot study. J Am Osteopath Assoc. 1998;98:264–272.
10. Knebl JA, Shores JH, Gamber RG, et al. Improving functional ability in the elderly via the Spencer technique, an osteopathic manipulative treatment: a randomized, controlled trial. J Am Osteopath Assoc. 2002;102:387–396.
11. Hartman SE, Norton JM. Craniosacral therapy is not medicine. Phys Ther. 2002;82:1146–1147.
12. Korthals-de Bos IB, Hoving JL, van Tulder MW, et al. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: economic evaluation alongside a randomised controlled trial [electronic version]. BMJ. 2003;326:911.
13. Ventegodt S, Merrick J, Andersen NJ et al. A Combination of Gestalt Therapy, Rosen Body Work, and Cranio Sacral Therapy did not help in Chronic Whiplash-Associated Disorders (WAD) - Results of a Randomized Clinical Trial. ScientificWorldJournal. 2005;4:1055-68.
14. Licciardone JC, Stoll ST, Fulda KG, et al. Osteopathic manipulative treatment for chronic low back pain: a randomized controlled trial. Spine. 2003;28:1355-62.
15. Wilson E, Payton O, Donegan-Shoaf L, Dec K. Muscle energy technique in patients with acute low back pain: a pilot clinical trial. J Orthop Sports Phys Ther. 2003;33:502-12.
16. Guiney PA, Chou R, Vianna A, et al. Effects of osteopathic manipulative treatment on pediatric patients with asthma: a randomized controlled trial. J Am Osteopath Assoc. 2005;105:7-12.