Coding case study - OMT Codes for use by DOs and MDs
Article by Angelia Halaja-Henriques, PAFP Communications Director
Credit: Note this article was directly taken from the Pennsylvania Academy of Family Physicians website at www.pafp.com/MMS/coding and the material posted below and even more information can be obtained by visiting the PAFP website at http://www.pafp.com/.
Pennsylvania Academy of Family Physicians
2704 Commerce Drive,
Suite A, Harrisburg, PA 17110
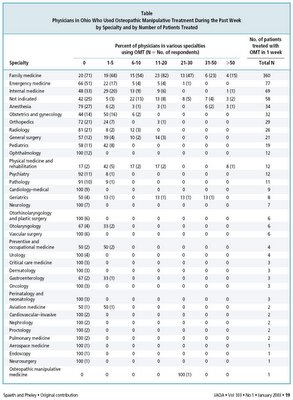
OMT has value for patients & docs. Positive outcomes helped to establish Osteopathic Manipulative Treatment (OMT) within the federal codes and eventually to become recognized in the CPT Manual 11 years ago.
Reasons why osteopathic family physicians with training in OMT should make it part of their practice today include the offer of holistic treatment, more satisfying patient encounters and an economic boost. Family physicians who practice manipulation say it is rewarding, effective and tout the value of the “laying on of hands.”
Note that OMT is not therapy; OMT is a treatment option by definition and in practice and is reimbursable as such. OMT also is not the same as chiropractic therapy; there are distinct codes for OMT vs. chiropractic manipulative therapy (CMT). Note too that the AMA CPT coding manual clearly states that code descriptions are in no way intended to be specialty- or profession-limiting. Therefore, an MD or DO can do CMT.
The economic incentive comes from the CPT guideline that a patient visit and OMT can both be billed at the same visit using modifier –25. This is not to say that all payors honor the guideline.
It’s a gray zone,” said Dr. Williams, who maintains a private practice while serving as a medical director for Capital Blue Cross in the midstate. Many payors like Capital Blue Cross take a hard line on the usage of modifier –25, referring to its original definition as a “significant, separately identifiable E/M service by the same physician on the same day of the procedure or other service.” They mistakenly see the office visit as preservice work for the procedure.
These payors are missing the clarifications made over the years, including one in CPT 1999 that “the E/M service may be prompted by the symptom or condition for which the procedure and/or service was provided. As such, different diagnoses are not required for reporting of the E/M services on the same date.” The clarification was published specifically because private payors were and are bundling E/M and OMT codes. The separate nature of E/M from OMT also was supported within recommendations implemented in 2004.
When asked about bundling, PAFP General Counsel Charles Artz, Esq. took an equally hard line. He wrote that the opinion of the AMA CPT Assistant is that “it’s absolutely NOT PART OF THE PRESERVICE WORK.
“The E/M code always may be billed separately with a -25 modifier,” he continues, “Is there any wonder there’re class action lawsuits?”Artz cites the HIPAA Transaction and Code Set standard as the statutory framework requiring payors to honor the CPT codes, code descriptors and modifiers. He has successfully employed his argument in court. “Under federal law,” says Artz, “[CPT codes] are the exclusive coding rules, to the exclusion of all other rules and interpretive guidelines.” Additionally, he says, “official comments make clear that modifiers are included in the code set, but that code sets do not include all operational guidelines or instructions.”
Further evidence against bundling is the minimal relative value unit (RVU) assigned to OMT which sets the Medicare physician fee for the procedure. The work RVU for OMT code 98925 is 0.45. According to the AOA, the OMT codes are valued only for the actual work of the procedure. “This is the same work value as code 99212,” says AAFP Coding & Compliance Specialist Cindy Hughes, CPC. “Obviously when payors say that there is preservice work included in the OMT codes, they are not accounting for much.”
The issue of pre- and postservice work being included in the code can be confusing for payors. Many other procedures and services include pre- and postservice work, and CMT specifically includes” pre-manipulation patient assessment.”
While bundling is prevalent across the country and is an advocacy issue of the American Medical Association and AOA, some family physicians are getting paid for both the E/M and OMT. Sam Schrack, DO, (Williamsport) provides manipulative treatment about once or twice a week and has not had trouble getting reimbursed using the –25 modifier. A family physician with an emphasis in sports medicine, Michael Cordas, DO, (Harrisburg) also reports no OMT reimbursement problems. Dr. Cordas qualified his statement by adding that he uses OMT as an “adjunct treatment and then very selectively.”
The AOA suggests physicians negotiate to add the following language into their payor contracts: “MCO agrees to adhere to the CPT codes, including notes, guidelines and instructions printed within the codebook and agrees not to bundle payment codes unless the edit conforms to the attached fee schedule and CPT. (Attach a fee schedule for the OMT and E/M codes- use the fees the physician expects to be paid.) In addition, MCO agrees to respect the CPT modifier –25 when used with an office visit and a procedure such as OMT when performed on the same day. (or in the alternative, “MCO agrees to pay E/M and OMT as Medicare does.”) Also, MCO warrants that each payor subject to this agreement conform to the fee schedule and these provision.”
OMT as a capitated service
Including OMT in capitation is another one of the primary reimbursement problems physicians may encounter.
“OMT should not be subject to capitation. It’s a separate procedure, separately payable,” says Artz.
Careful review of managed care contracts will tell physicians whether OMT is capitated with other services. Physicians are encouraged to read the contract themselves or ask a health law attorney to do so as some payors do not properly interpret or communicate the exact nature of the capitation agreement.
Physicians and their attorneys are encouraged to renegotiate contracts to exclude OMT from capitation or increase the per patient fee over what is being offered physicians who do not perform OMT. If a physician can carve out OMT from capitation, the AOA suggests including a list of OMT codes that will be paid fee for service.
Studies show the efficacy and efficiency of OMT, so it is worth the time of both the payor and physician to renegotiate for fee for service.
Covered treatment?
Dr. Schrack warns that patients’ policies might not cover OMT. If OMT is not covered, he suggests asking payers about billing the patient for the service. Dr. Williams also suggests encouraging patients to check caps on manipulation visits.
Appeal denials of correctly coded OMT visits
Similarly, it is worth a physician’s time and effort to resubmit denials and educate payors on correctly applying CPT codes related to OMT. One PAFP member found that payers started approving codes previously denied after his practice called to question denials.
CPT & ICD codes
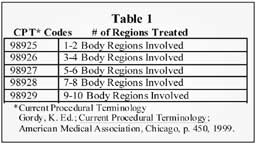
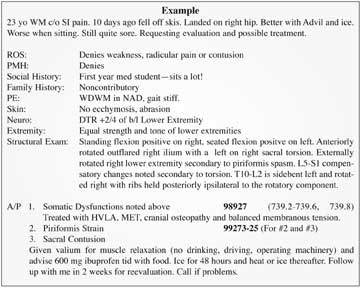
The procedure codes for OMT relate to the number of regions affected and the diagnosis codes to the specific region(s) affected.
OMT CPT codes [inpatient & outpatient]
98925
1-2 body regions
98926
3-4 body regions
98927
5-6 body regions
98928
7-8 body regions
98929
9-10 body regions
Body region codes:
head
sacral
rib cage area
cervical
pelvis
abdomen
thoracic
lower extremities
viscera region
lumbar
upper extremities
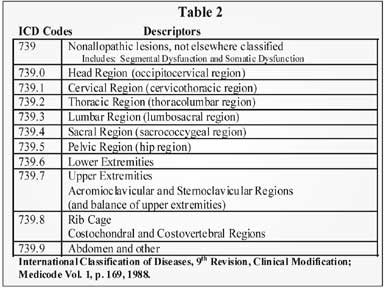
ICD Codes Descriptors
739._
Somatic dysfunction
739.0
Head region
739.1
Cervical region
739.2
Thoracic region
739.3
Lumbar region
739.4
Sacral region
739.5
Pelvic region
739.6
Lower extremities
739.7
Upper extremities
739.8
Rib cage
739.9
Abdomen and other
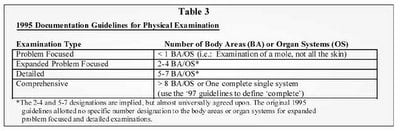
Be sure to thoroughly document the history, examination and medical decision making (MDM) to support an appropriate E/M code. While all physicians know not to supplement documentation to upcode, neither should they omit information from the history or exam that supplements the diagnosis process.
Physicians should document the history using CPT and their own clinical judgment. The note might include the chief complaint, history of present illness, a review of systems and any family, social and/or medical histories. The note also should use federal guidelines to detail the physical exam. The structural exam supports medical necessity for OMT, and the assessment and plan (A/P) can serve as procedure note and justify other interventions, such as pharmaceutical treatments.
If during MDM a physician sees a need for injections in addition to OMT, list these codes first as they are more complex. Typically, the procedure and ICD code are listed first followed by the E/M with –25 modifier. Practices should consult payors for their specific preference.
Physicians are not limited in the number of dysfunctions that may be diagnosed, treated and/or billed. Physicians should include their notes and be specific about physical findings to limit misunderstanding by the payor. Submitting detailed notes also supports coding when there is not enough room on the payor form for what are often many ICD codes.
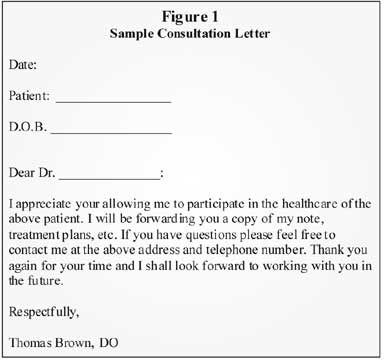
Physicians trained in OMT also may do consults.
AOA coding case study
A 42-year old male with confusion and pain in the neck and upper back presents to a neurosurgeon. Patient also complains of exacerbation of previous lumbar disc herniation with radiculitis following a motorcycle accident. After evaluation of the patient, the diagnosis is: (1) closed head injury and (2) somatic dysfunction of the head, cervical, lumbar, sacral and rib region. The physician then utilizes osteopathic manipulative treatment to treat the patient’s head, cervical, lumbar, sacral and rib regions.
Diagnosis Coding
Somatic dysfunction, head 739.0
Somatic dysfunction, cervical 739.1
Somatic dysfunction, lumbar 739.3
Somatic dysfunction, sacral 739.4
Somatic dysfunction, rib 739.8
Procedure Coding
Osteopathic manipulative treatment (OMT); five to seven body regions involved 98927
Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three key components:
a detailed history
a detailed examination
medical decision making of moderate complexity 99214-25
Explanation of Code Selection
For the diagnosis coding of somatic dysfunction it is necessary to code to the fourth digit (e.g. 739.1) as one should code to the most specific ICD-9 code. Not coding to the fourth digit could cause the payor to reject this claim. Code 98927 was selected for the OMT provided as five regions were treated. In selecting the E/M code, since the patient had been seen by the physician within the past three years, this was an established patient. A detailed history and examination were performed and medical decision making of moderate complexity was provided, hence the selection of CPT code 99214. The –25 modifier was added as this indicates to the payor that a significant, separate identifiable evaluation and management service was provided in addition to the OMT.
Expert Q & A
Cindy Hughes, CPC, is a Coding & Compliance Specialist with AAFP.
Q: How would a physician code injections in addition to OMT? Are there specific codes and/or modifiers?
A: Ms. Hughes: The National Correct Coding Initiative (NCCI) edits from CMS bundle injections including lumbar epidurals into the OMT codes. If an injection is a distinct procedural service such as an unrelated joint injection or trigger point injection, a –59 modifier should be appended to the code for the lesser procedure.
Chapter 11 of the NCCI for Medicare Part B Carriers states: “Osteopathic Manipulative Treatment is subject to Global Surgery Rules. Per Medicare Anesthesia Rules a provider performing OMT cannot separately report anesthesia services such as nerve blocks or epidural injections for OMT. In addition, per Medicare Global Surgery Rules, postoperative pain management after OMT (e.g., nerve block, epidural injection) is not separately reportable. Epidural or nerve block injections performed on the same date of service as OMT and unrelated to the OMT may be reported with OMT using modifier –59.”
Q: What’s the difference between the –51 and –59 modifiers? Can you give an example of how to use each related to OMT?
A: Ms. Hughes: The –59 modifier is used to show that two codes which are listed in the NCCI edits as being bundled or exclusive are being appropriately billed due to a distinct procedural service. The –51 modifier is used to indicate multiple procedures. A patient might come to the office for scheduled procedures such as lesion removals and ask for an osteopathic treatment before the surgical procedures. For instance, the patient is scheduled for excision of benign lesions of the arm and leg but has back pain and requests an OMT service as well: codes could be 11403, 11402-59-51 and 98925-51.
Sources
All contents © 2000 Pennsylvania Academy of Family Physicians. All Rights Reserved.
OMT Coding Strategies To Boost Your Bottom Line; Implement these strategies for better OMT reimbursement. Douglas J. Jorgensen, DO, CPC. Osteopathic Family Physician News. Osteopathic Principles and Procedures - April, 2004. http://www.acofp.org/member_publications/0404_1.html
Consistency Counts for OMT Coding; Osteopathic family physicians need to be both highly skilled in medicine and practice management. Douglas J. Jorgensen, DO, CPC. Osteopathic Family Physician News. April, 2003. http://www.acofp.org/member_publications/0403_coding.html
Osteopathy: OMT Codes. http://www.drfeely.com/doctors/osteo_coding_1.htm
Osteopathic Physicians, Bundling And Modifier -25, Issue Paper: Reimbursement of Osteopathic Manipulative Treatment, Osteopathic Coding, American Osteopathic Association, Division of Socioeconomic Affairs