Last Updated on July 21, 2022 by Laura Turner
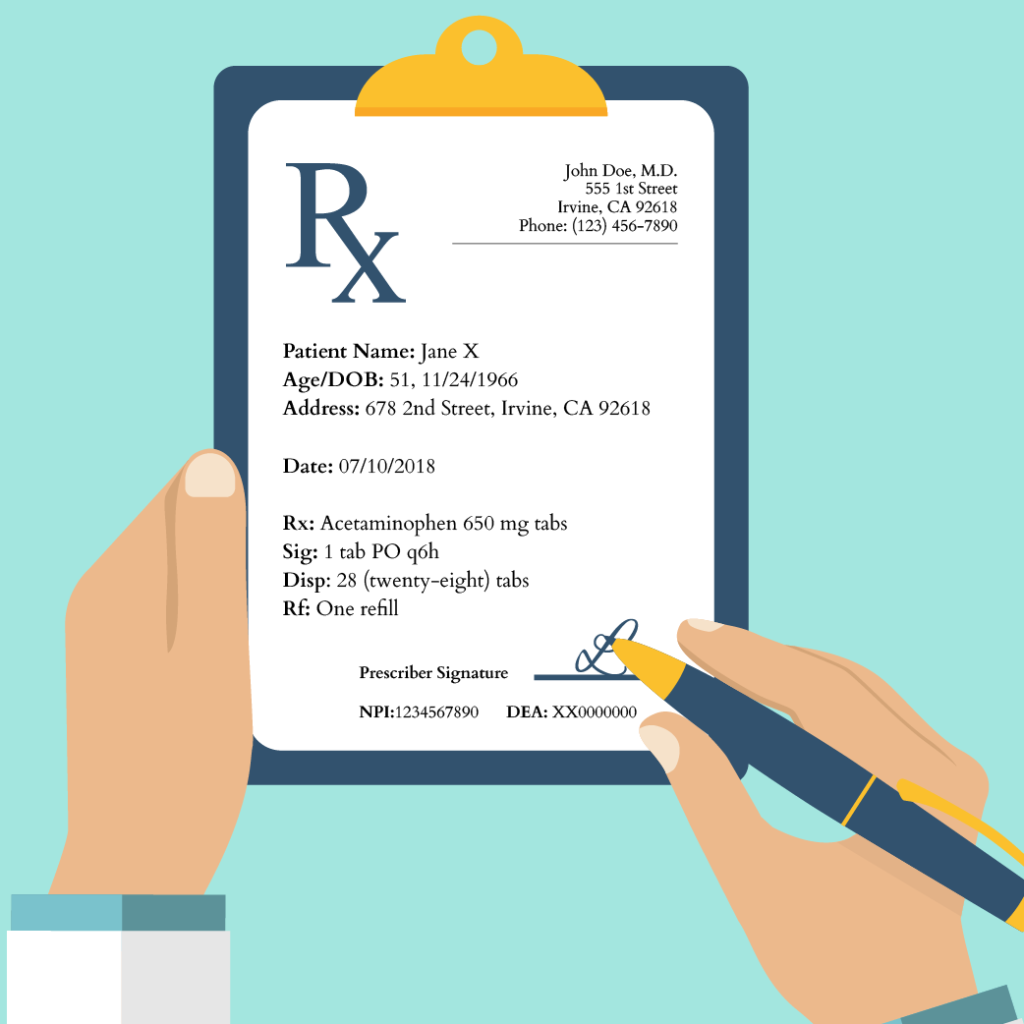
Are you learning to write a prescription? It’s not that difficult once you know the seven steps to write a prescription safely. Every drug prescription consists of seven parts: the prescriber’s information, the patient’s information, the recipe (the medication, or Rx), the signature (the patient instructions or Sig), the dispensing instructions (how much medication to be dispensed to the patient or Disp), the number of refills (or Rf), and the prescriber’s signature (including his or her National Provider Identifier and/or Drug Enforcement Agency number). Below are each of these sections in detail.
Time needed: 3 minutes
How to write a prescription in 7 steps:
- Prescriber’s Information
This information is usually found at the top of the prescription. It generally consists of the prescribing clinician’s name, office address, and contact information (usually the office’s telephone number).
- Patient’s Information
Below the prescriber’s information is the patient’s information. This section will include the patient’s full name, age, and date of birth. Sometimes the patient’s home address will be found here, as well. You should also specify the date you wrote the prescription.
- Recipe (Rx)
The recipe should include the medication being prescribed, its dose, and its dosage form. For example, if you are prescribing 650 milligrams (mg) tablets of acetaminophen, you would write “acetaminophen 650 mg tablets” or “acetaminophen 650 mg tabs.”
- Signatura (Sig)
After the recipe is the signature, the signature (Sig) gives the patient instructions on how to take the medication. The Sig should include information on how much drug to take, how to take it, and how often to take it.
For example, if you would like your patient to take one 650 mg tablet of acetaminophen every six hours, you would write “Take 1 tablet by mouth every six hours” or, using abbreviations, “1 tab PO q6h.”
For as-needed or pro re nata (PRN) prescriptions, you should indicate that the prescription is PRN and describe the conditions under which your patient can take the prescribed medication. Writing your prescription as a PRN order essentially gives the patient the option to take the drug when needed.
Let’s say that you would like your patient to be able to take one 650 mg tablet of acetaminophen every six hours when he or she has a headache. In that case, your instructions would read, “Take 1 tablet by mouth every six hours as needed for a headache” or “1 tab PO q6h PRN headache.” - Dispensing Instructions (Disp)
Next comes the dispensing instructions, which let the pharmacist know how much medication you would like your patient to receive. You should include the amount of medication you would like to be dispensed and the form in which it should be released. You should also make sure to write out any numbers you use here to minimize the risk of a medication error. For our acetaminophen example, if you would like your patient to receive a one-week supply (or 28 tablets) of the medication, you would write “28 (twenty-eight) tablets” or “28 (twenty-eight) tabs.”
- Number of Refills (Rf)
After the dispensing instructions, specify how many times you would like your patient to refill his or her medication. Be sure to write out again any numbers you use. If you do not want to prescribe any refills, write “zero refills.” For our hypothetical acetaminophen example, if you are prescribing one refill, you would write “1 (one) refill.”
- Prescriber’s Signature
At the bottom of the prescription, you should sign your name. Oftentimes, you will include your National Provider Identifier (NPI) in this section. For controlled substances, you usually will include your Drug Enforcement Agency Number. These are necessary for the pharmacy to verify your prescription more easily.
So for our hypothetical acetaminophen example, our prescription looks like this:
In 2020, over four and a half billion prescriptions were filled at pharmacies across the United States. Given their sheer prevalence, prescriptions are a key source of medical errors. In fact, prescription errors account for 70% of medication errors that result in harm. Thus, it is crucial that all clinicians master the ability to properly write a prescription.
In learning to write a prescription properly, it is worth discussing two common sources of prescription errors. First, if you are handwriting your prescription, make sure that it is legible. While e-prescribing is increasingly making handwritten prescriptions a thing of the past, you will likely have to manually prescribe medications at some point in your career. Illegible prescriptions are a source of frustration for patients, pharmacists, and other medical providers, and can increase the risk of medication errors. No matter how busy you are, it is always better to spend a few extra seconds slowly writing out a legible prescription than risk your patient’s health.
Always be cautious when using abbreviations. While abbreviations are commonly used in medicine, you should keep in mind that the risk of a medication error is increased when abbreviations are ambiguous or misused. So if you choose to use abbreviations in your prescriptions, be sure only to use well-known ones (commonly used medical abbreviations can be found here). If you are unsure whether you should use an abbreviation, spend the extra few seconds to write out your directions completely.


Great overview of prescriptions. My significant other is a pharmacist, and he always stresses the importance of CLEAR prescription information from the physician.